What is MDLD?
Mine dust lung disease (MDLD) is a broad term used to identify a range of work related lung diseases caused by exposure to harmful levels of respirable dust at mines and quarries.
These diseases are progressive, meaning they can get worse over time, and normally take at least 10 years of prolonged dust exposure to develop and produce symptoms.
In some cases, workers can get early signs of disease sooner. This can be due to the level of dust, but also individual susceptibility. The longer a person is exposed to harmful levels of respirable dust, the more serious and life-altering the disease becomes.
The good news is that limiting exposure to respiratory hazards, especially respirable dust, can stop the progression of the disease from its early stages.
What is respirable dust?
When it comes to dust, size matters.
The dust particles created by mining fall into two size categories, each with different effects on the human body.
It’s exposure to high volumes of ultra-fine respirable dust over an extended period of time that can lead to the development of mine dust lung disease.
| Description | |
|---|---|
Inhalable dust (about 0.1mm or 100µm diameter) |
|
Respirable dust (about 0.005mm or 5µm diameter) |
|
Types of MDLD
Respirable dust exposure at mines and quarries can cause irritation to the eyes, skin and respiratory tract, and prolonged exposure can lead to a range of mine dust lung diseases including:
- pneumoconiosis
- coal workers’ pneumoconiosis (CWP)
- mixed dust pneumoconiosis (MDP)
- silicosis
- asbestosis
- chronic obstructive pulmonary disease (COPD)
- chronic bronchitis
- emphysema
- lung cancer.*
*Lung cancer may also have non occupational causes, but may be caused by carcinogens in the mine atmosphere including respirable silica dust, diesel exhaust emissions and welding fumes.
Pneumoconiosis
Pneumoconiosis is an occupational form of pulmonary fibrosis that causes scarring of the lungs. The type of pneumoconiosis depends on the type of dust exposure. For example, coal workers’ pneumoconiosis is caused by coal dust and silicosis from crystalline silica.
Pneumoconiosis may take several years to develop, commonly 10 years or more, and the disease can manifest in different people in different ways, depending on the composition of the dust, the duration of exposure and other individual factors.
The severity of the disease can be described as either simple or complicated. Simple forms of the disease can progress to complicated forms if harmful levels of dust exposure continues.
Complicated pneumoconiosis is also known as progressive massive fibrosis or PMF.
| Simple | Complicated | |
|---|---|---|
| Biology |
|
|
| Progression |
|
|
| Prognosis |
|
|
Limiting exposure to respirable dust can stop the development of the disease in its early stages.
Coal workers’ pneumoconiosis
Coal workers’ pneumoconiosis (CWP) is a type pneumoconiosis caused by long-term occupational exposure to harmful levels of respirable coal dust.
Silicosis
Silicosis is caused by respirable crystalline silica. Silicosis can develop faster than CWP and is considered more dangerous, as crystalline silica is known to cause lung cancer.
The main types of silicosis are:
- acute silicosis which can develop following very heavy exposure to silica within weeks or years of exposure. In this type of silicosis the lungs fill with fluid which causes severe breathlessness
- accelerated silicosis is linked to high exposure of silica. There is rapid increase in scarring of the lungs within 10 years of first exposure
- chronic silicosis is the most common form of the disease. Scarring of the lungs occurs slowly over 10-30 years after first being exposed.
Like CWP, silicosis may also be characterised as simple or complicated.
How MDLDs develop
The longer the exposure, the more serious and life-altering disease can become.
The basics
Under normal conditions, the lungs defensive mechanisms can remove small quantities of respirable dust. But when exposed to a high volume of dust, the removal process may cause damage to the fine structures in the alveolar spaces. Some particles can become trapped in the tissue, causing irritation and triggering a response from the immune system.
Immune cells repeatedly try to heal the irritated area and small scars begin to form. This is called fibrosis. If enough scar tissue forms, lung function can be reduced.
The collections of dust and scarring may later show up as small round nodular shapes on a chest X-ray.
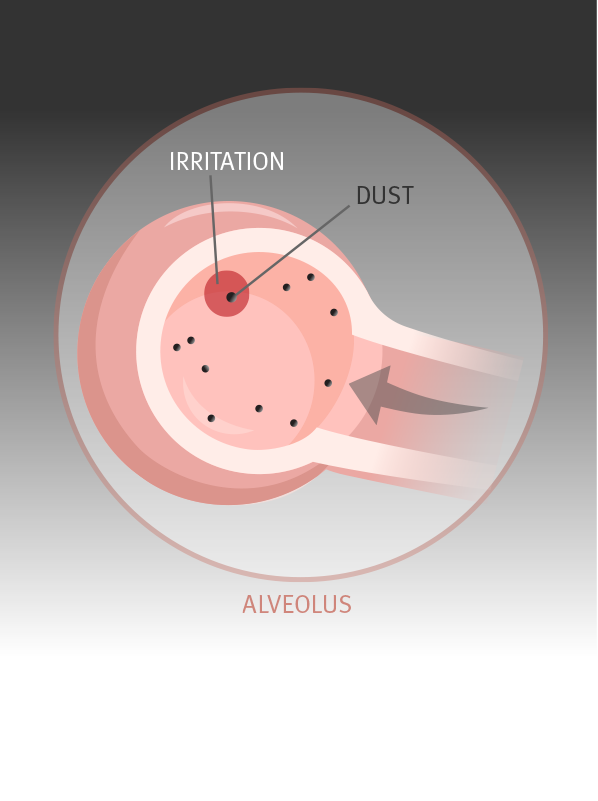
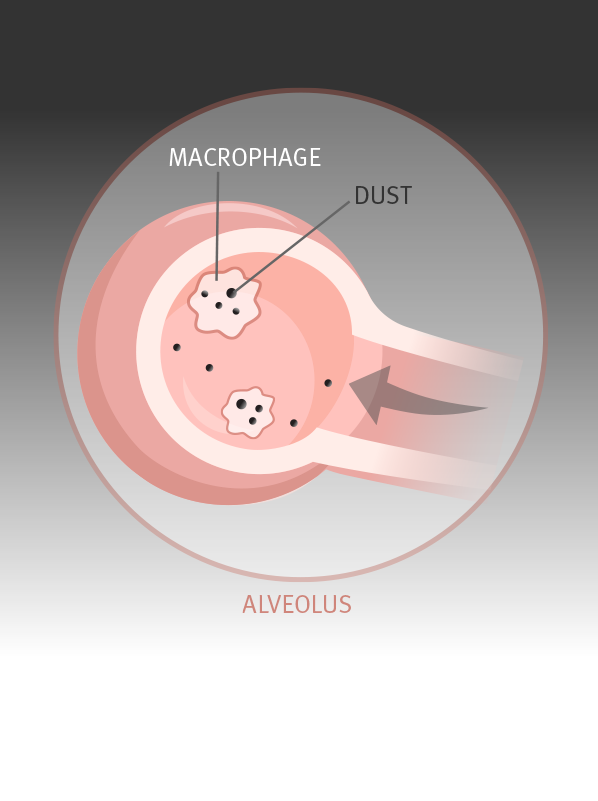
The following images show how mine dust lung diseases like coal workers’ pneumoconiosis and silicosis develop.
The details
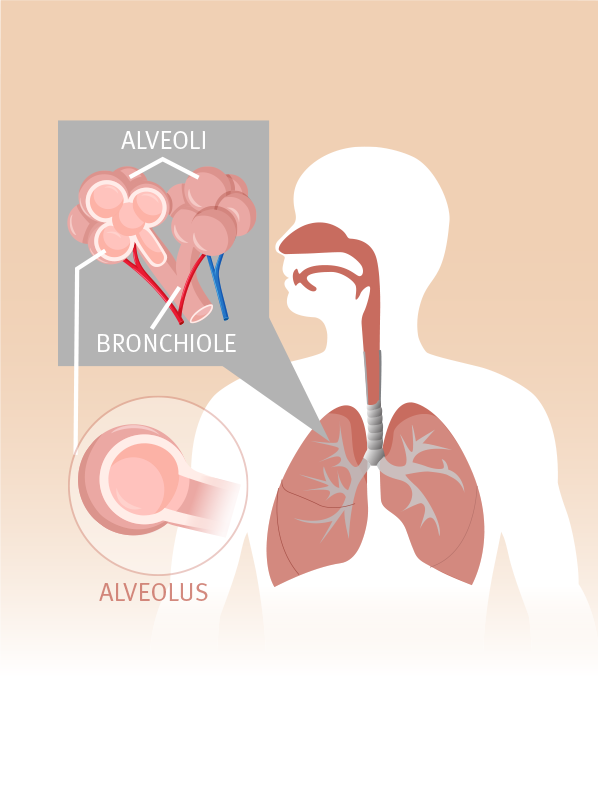 Alveoli are tiny air sacs responsible for exchanging oxygen and carbon dioxide with the blood. A typical pair of lungs contain approximately 700 million alveoli. Alveoli are tiny air sacs responsible for exchanging oxygen and carbon dioxide with the blood. A typical pair of lungs contain approximately 700 million alveoli.
| 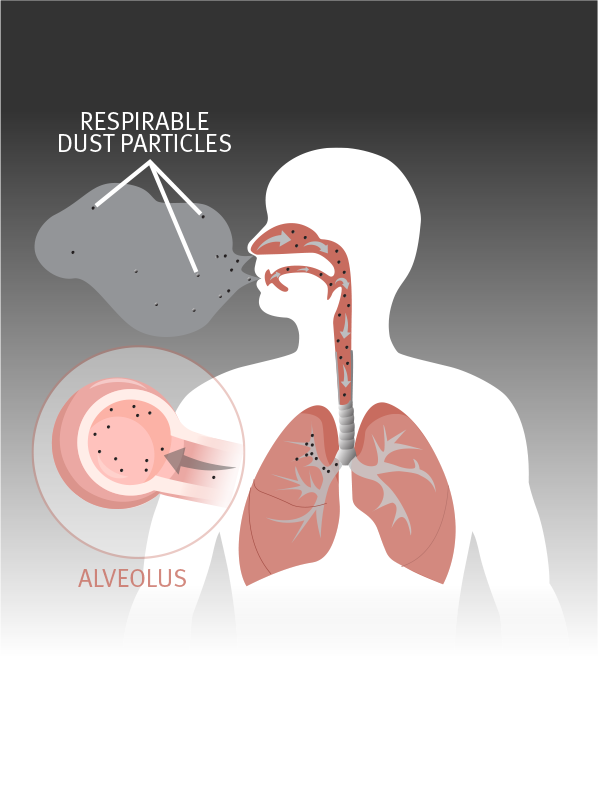 Because respirable dust particles are so small, they’re able to travel all the way into the alveoli, where they can cause irritation inside the air sac. Because respirable dust particles are so small, they’re able to travel all the way into the alveoli, where they can cause irritation inside the air sac.
|
 In response to the dust particles, the lung’s defence mechanism kicks in. Macrophages, a type of white blood cell, engulf the dust particles to destroy or clear them away. In response to the dust particles, the lung’s defence mechanism kicks in. Macrophages, a type of white blood cell, engulf the dust particles to destroy or clear them away.
|  They send out chemicals to attract more macrophages and other similar types of cells. They work together to engulf and clear the dust particles. They send out chemicals to attract more macrophages and other similar types of cells. They work together to engulf and clear the dust particles.
|
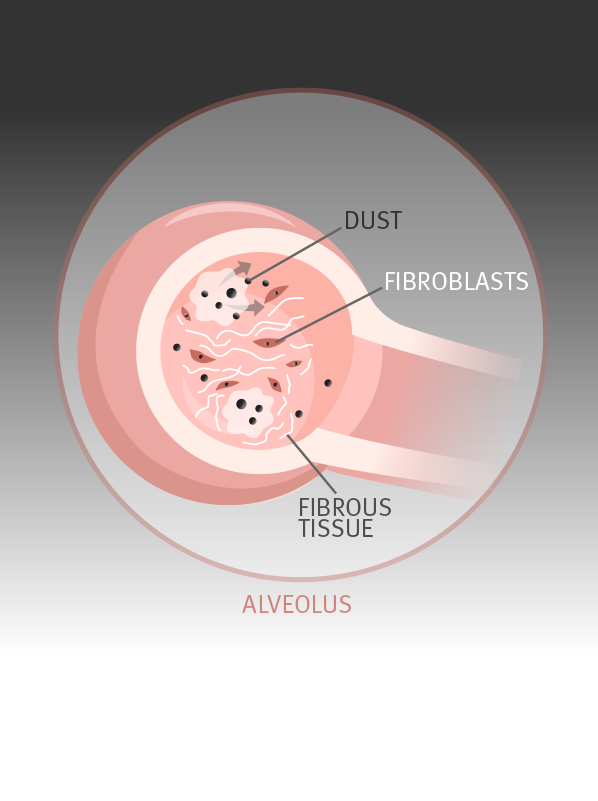 If the concentration of dust is too high, a wider immune response is triggered by the macrophages. Fibroblast cells produce collagen to form nodules of scar tissue around the particles in an attempt to trap the coal-laden macrophages. If the concentration of dust is too high, a wider immune response is triggered by the macrophages. Fibroblast cells produce collagen to form nodules of scar tissue around the particles in an attempt to trap the coal-laden macrophages.
| 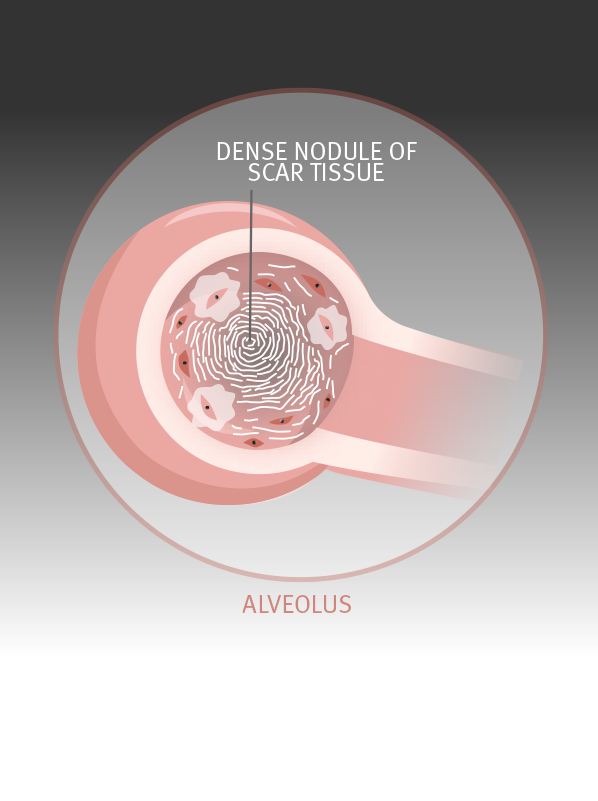 Over time, with continued overexposure to respirable dust, the process repeats many times and more nodules of scar tissue form. Over time, with continued overexposure to respirable dust, the process repeats many times and more nodules of scar tissue form.
|
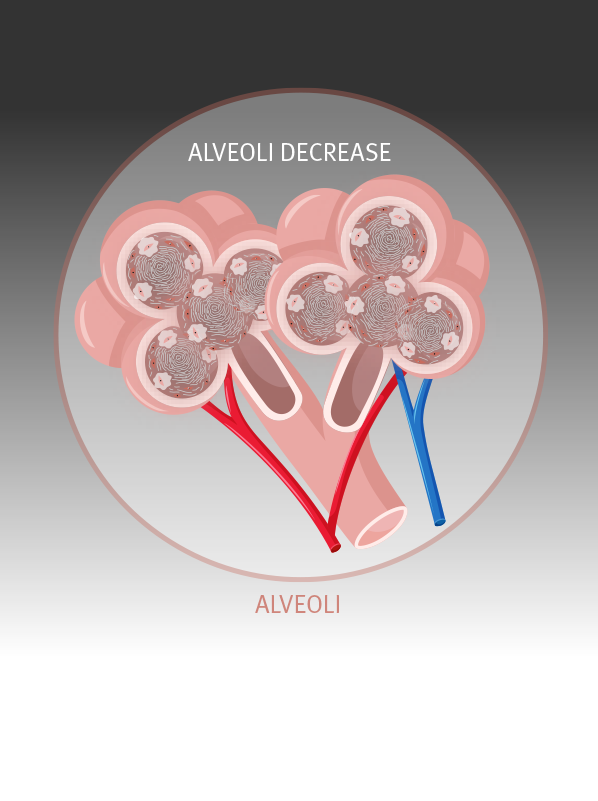 Overcome with scar tissue, the alveoli become unable to function normally, reducing the transfer of oxygen into the bloodstream. Overcome with scar tissue, the alveoli become unable to function normally, reducing the transfer of oxygen into the bloodstream.
| 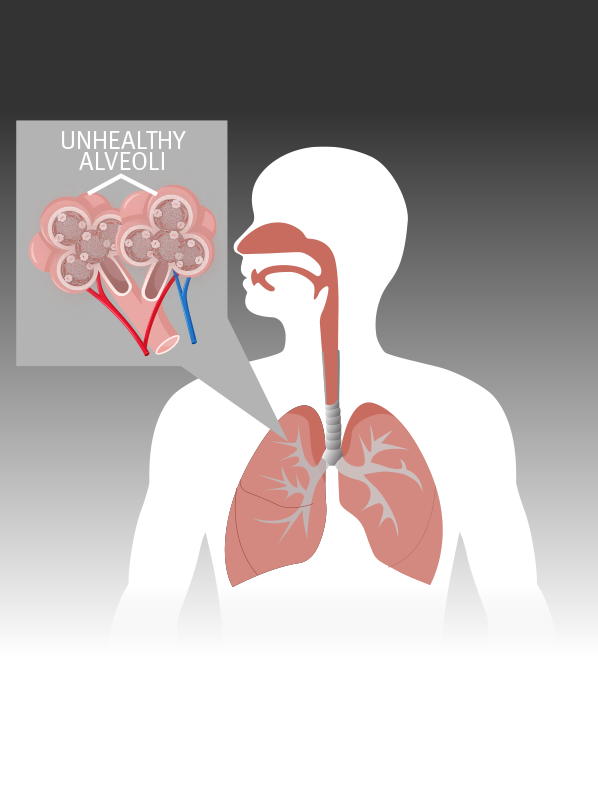 With continued overexposure to respirable dust, the scarring becomes so extensive that it becomes hard to breathe deeply. The amount of oxygen entering the bloodstream is also reduced. With continued overexposure to respirable dust, the scarring becomes so extensive that it becomes hard to breathe deeply. The amount of oxygen entering the bloodstream is also reduced. |
Chronic obstructive pulmonary disease
Mine and quarry dust exposure can also cause chronic obstructive pulmonary diseases (COPD) such as emphysema and chronic bronchitis. These diseases differ from pneumoconiosis in how they damage the lungs. Instead of causing nodular scars, the air passages and air sacs of the lungs become inflamed and damaged.
Tobacco smoking also causes COPD. If a mine or quarry worker also smokes tobacco, both the dust and tobacco smoke may add to the worker’s lung damage.
Symptoms
In the early stages of the disease, workers may have either no obvious symptoms or mild symptoms such as chronic cough or occasional shortness of breath.
As the diseases progress, workers will demonstrate some or all of these symptoms:
- shortness of breath on exertion and eventually at rest
- chronic cough
- chronic chest infection
- sputum – this will be black for CWP
- lung dysfunction
- pulmonary hypertension
- heart problems.
Risk factors
Quitting smoking is one of the most important things you can do to protect yourself.
Anybody exposed to harmful levels of respirable dust is at risk of developing a dust-related lung disease. Your risk level is directly linked to your total level of exposure and some personal risk factors.
Exposure level
Mine dust lung diseases are caused by exposure to harmful levels of respirable dust over a long period of time. It’s important to remember that under normal conditions, your lungs’ defence systems can easily handle respirable dust particles.
Frequent exposure to high concentrations of dust can overwhelm the defence system, causing the development of scarring or other damage. You will not develop disease after one shift of high exposure. It takes years for dust build up in the lungs to cause the onset of the disease.
For a full overview of workplace exposure risks, read about MDLD prevention.
Personal risk factors
It is unclear why some mine workers develop mine dust lung disease, and others don’t, even if they are exposed to the same working conditions. Research to date has shown that workers who have had tuberculosis, or have a family history of rheumatoid arthritis, may be more likely to develop a mine dust lung disease.
Smoking has been established as a factor that increases the risk of developing or accelerating disease. Quitting smoking is one of the most important things you can do to protect yourself.
Why do doctors advise mine and quarry workers exposed to dust to stop smoking?
Smoking interferes with the lung’s ability to clear dust which increases the risk of getting a mine dust lung disease.
Mine and quarry dust and tobacco smoke exposure both cause emphysema (an obstructive disease of the lung).
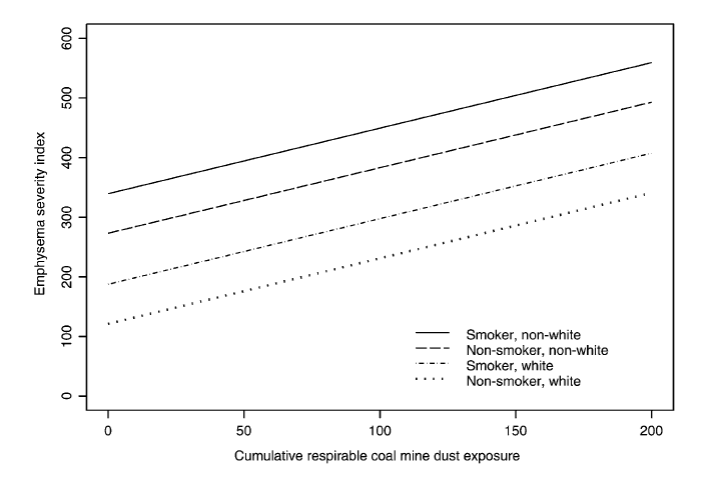
A study by the US National Institute for Occupational Safety and Health (NIOSH) found that cumulative coal dust exposure and cigarette smoking each increased the severity of emphysema. However, the study could not tell whether the obstructive lung disease was caused by coal mine dust or by smoking.
The graph shows that exposure to coal dust increases emphysema (destruction of lung tissue) faster in smokers than in non-smokers.
Treatment and management
If you have early stage disease, avoiding further exposure to harmful levels of dust and irritants (like cigarette smoke or diesel exhaust emissions) may stabilise the disease. You should also improve your general respiratory health through exercise and diet programs.
If your case is more advanced, treatments will generally be aimed at limiting further damage to the lungs, managing symptoms and improving quality of life. Treatments include:
- quitting smoking
- pulmonary rehabilitation including:
- specialised exercise and diet program
- breathing techniques/managing breathlessness
- oxygen therapy to ease shortness of breath
- bronchodilator medication, like those used to treat asthma
- immunisations to avoid infection.
In more serious cases of disease, lung transplants have been successfully performed.
For more information on pulmonary rehabilitation, speak to your respiratory physician or visit the Lung Foundation Australia website.


